People Bodies
In Pursuit of Fertile Ground: Continuing IVF When the Odds Are Against You
I am at the nether reaches of my fertility, curious as to what I can still grow. This remains a shock.
My conversation with Yolanda lasted less than sixty seconds—long enough for her to say “abnormal” and “I am sorry,” and “it sounds like you have a plan in place.” Dr. Hertz left me a message a few hours later. She said, “I know you got a call from us today and I just wanted to see if . . . well, we have a plan, so if you have questions about the test results, just give me a call.”
Every part of the in-vitro fertilization process, before Yolanda’s call, had defied my expectations. I have few eggs, and yet we retrieved two that were mature. Odds of fertilization were lower given the small number of eggs, and yet we had an embryo that was, as Dr. Hertz had said, “developing nicely.” When I returned to the clinic six weeks later—time enough to note the many freedoms I have with time, money, and spontaneity in not having children—a feeling of purpose renewed, without my particular encouragement. I did not meditate or focus on positive thinking before returning. I did not consciously restore my reserves of optimism or forbearance.
Yet between the time I stepped from the elevator into the waiting room of the clinic, typed my name and date of birth on the touchscreen monitor to the right of the reception desk, selected Dr. Hertz’s name from the list of eight doctors in the practice, then selected IVF and Cycle Monitoring Bloods/Ultrasound , I once again felt a sense of possibility. As a friend had said, when I described this feeling, “Well, that’s the addiction—to the possibility it will work.”
I had a blood test to check my progesterone level, which would indicate if I had ovulated yet that month—if I had, I would start wearing Estradiol, a thin patch that secretes estrogen into the body. It’s a primer, with the hopes that next month more follicles will mature.
And it worked: My first ultrasound after a week on the hormones reflected four well-developed eggs, two burgeoning eggs, and more dark flecks, which the attending physician called, “the next cohort.” We retrieved six eggs on a Friday, and on Saturday, a nurse called to tell me we had five embryos, a surreal and enchanting concept. I lay down, exhilarated—I felt like I could rest.
*
My doctor, I feel, has never once misled me. I am forty-two. Without intervention, I have an 11 percent chance of presenting a good quality egg each month. With help, we need to retrieve at least ten eggs a cycle for the odds to be in our favor. On many occasions, Dr. Hertz has reiterated, “It’s a numbers game.”
In a personal health piece for The New York Times in 2016, Jane Brody quoted Dr. Mark V. Sauer, former director of the IVF Clinic at the New York Presbyterian/Columbia University Medical Center; Sauer recognized that many women want to wait to conceive until their careers are established and they are in secure relationships. However, he explained, “ages thirty-five to forty-five represent the ‘terminal decline in normal fecundity,’ as well as a greatly increased risk of producing eggs and embryos with chromosomal and other abnormalities.”
The habit of unquestioning faith forms nonetheless—perhaps it has to, for one to commit. But though each step of the process can feel like a triumph, the only real triumph is in feeling one’s way through an unfamiliar landscape. The numbers have not changed.
For me, it is a reckoning. At thirty-one, I committed to a bad relationship because, after I had invested some time, I feared not finding a new partner within my reproductive window if I broke it off. By thirty-one, it seems, I already felt old. Four years later, the relationship had gone nowhere, and I ended it. I met my husband, Derek, that same year, but by then my priorities were stability and companionship.
It has taken time for places of solidity to form in the nebulous and, at times, painful transition between youth, fledgling adulthood, and real adulthood. I was forty-one when I mentioned to my gynecologist that my husband and I intended to have a baby. The fact of my age, and what that really meant for my fertility, had not landed yet. She said, “Make an appointment with a reproductive endocrinologist now. Today. It’s likely not too late, but you may need help.”
*
Joshua Tree National Park / photo by Derek Wright
A week after the second egg retrieval, a nurse called to say that two of the five embryos had grown enough to be biopsied. And then, while we were hiking the Mastodon Peak trail in Joshua Tree National Park—a trail which winds steeply uphill from the Cottonwood Spring oasis and which branches from the eight-mile Lost Palm Oasis trail, an endless and static up and down through the Colorado Desert toward an incongruous outcropping of California fan palms—my phone rang.
I was seated on a boulder while Derek ascended the craggy peak and waved to me from the top, seemingly weightless and agile, winding around the cluster of stacked boulders confidently and disappearing briefly on the other side of the peak. I’d made it 400 feet up a 476-foot climb. The recovery from the egg retrieval had been long and uncomfortable, and I felt ungainly and overweight. Derek is three years younger than me, but when I compared his energy and exuberance to my own fatigue and distraction, it felt like a ten-year age difference.
Yolanda was genial, but both embryos had abnormalities, a likelihood Dr. Sauer, and Dr. Hertz, had named for a woman my age. I told her I was prepared for it; I even laughed, and said, “ I am okay, I knew this was a possibility.” I thought, cynically, My eggs are expired .
The doctor has never misled me, but perhaps I have still been misled.
The visitors’ center on the western end of Joshua Tree National Park is not within park boundaries; it is four miles out, on Park Boulevard in the village of Joshua Tree. Inside, Derek and I wandered through a permanent exhibit on Joshua trees. I stared at the first panel, which read, What kind of a tree must be damaged to reproduce? What kind of tree relies on a moth for its seeds?
I knew that Dr. Hertz would call, and I felt relieved that when she did I did not have cell phone service; she had to leave a message: “I heard that you are on vacation. And I hope that you are having a good time. Call me when you can.”
The Mojave Desert is the only place in the world where the Joshua tree, which is really a rare yucca plant, thrives. The yucca moth pollinates Joshua trees, and lays her eggs inside of their flowers. Her larvae, when hatched, feed on the tree’s seeds. Botanist Elbert Little describes Joshua trees as “slow growing and long-lived.” Though their average lifespan is 150 years, they can reach 1,000 years of age, growing just a few centimeters each year, and, in some instances, not branching until twenty-one years have passed.
Joshua Tree National Park / photo by Derek Wright
I regarded these trees as I would a physique, or a silhouette, or a solo dancer on a stage—as spare and expressive. The bent limbs, to me, seemed held in freeze frame while recoiling from an electric shock. On some, every limb angled toward the sun. The shared reach of the limbs cantilevered the trunk, and the entire tree leaned sideways.
I predicted that Dr. Hertz would say there was no point in undertaking another cycle.
*
We speak when Derek and I are back in New York; the sameness of the desert landscape, the dusty trails and the afternoon heat, receding into memory. I sense she is hesitant to broach the discussion of next steps.
“It’s funny,” I say, “I was sitting on a boulder in Joshua Tree National Park, and it was the one place I had cell service.”
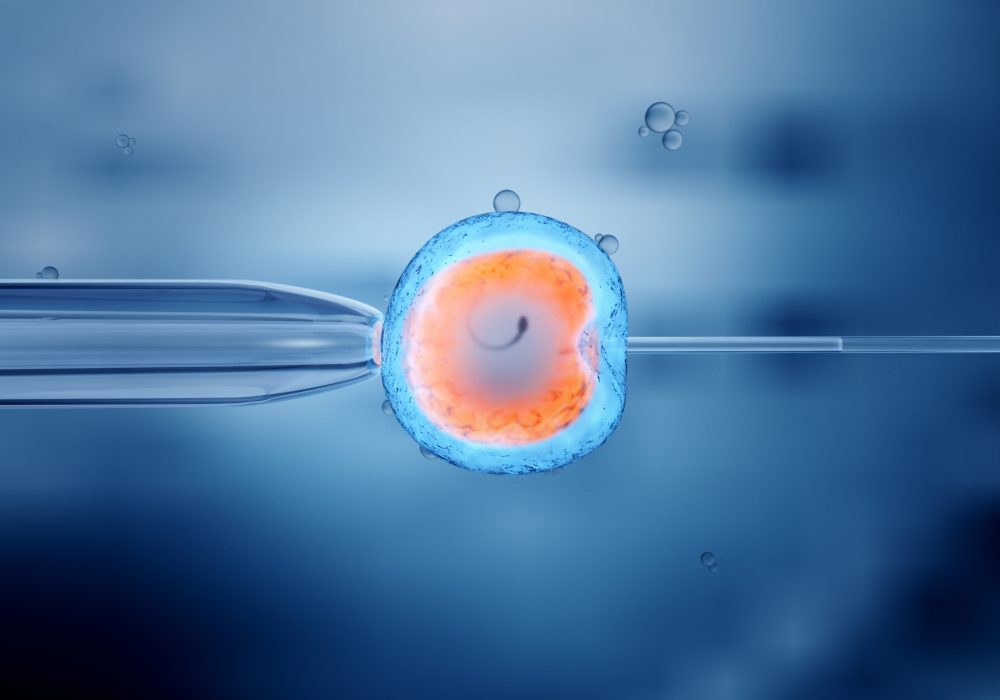
“How funny to be in such an otherworldly landscape while thinking about cooking up embryos!” the doctor says.
I hadn’t thought of it in such terms before. Now, however, I understand her point.
There are forty-four plant species within the park that are considered “rare,” among them Parish’s daisy, a radial flower with a bright yellow pistil and thin, fragile lavender petals. There are also 750 documented species of vascular plants and sixteen different cacti, including cushion foxtail cactus; chuckwalla, silver, matted, and pencil cholla; cottontop, Mojave mound, common fishhook, California barrel and hedgehog cactus; beavertail, dollarjoint, tulip, and grizzly bear prickly pear. According to the National Park Service, most plants would “literally cook” when exposed to the high temperatures in the park during the summer, but the teddybear cholla’s internal temperature often rises fifty-nine degrees or more above that.
I am at the nether reaches of my fertility, curious as to what I can still grow. This remains a shock, even as I consider a third IVF cycle, but it is also a fact that continues to assert itself.
The truth is, I like going to the clinic. That doctor’s office is no different than any other in that I am there to, in some way, care for myself. I chat with the nurses in the morning, when I go in for blood work, and in the afternoon, when one calls with the doctor’s instructions for the evening’s injections. Ultimately, it is only in writing that I can take the sum of our efforts and our options, and put some distance between the desert, a world of anomalies and unlikelihoods, and the rest of my life, where I feel safe enough to test such extremes.
*
Derek accompanies me to the clinic on a Saturday morning. I am at ease until Christina, the nurse set to draw my blood, steps away to read my case history. I can see her back, as she is at a standing monitor, one knee bent, the ball of one foot pressed into the floor. When she returns, several minutes later, I say, “So, you got the whole story.”
She says yes, and I realize we have never met. I am relieved, as I’d been anxious about seeing the regulars. I ask Christina to please use my right arm, as I have some nerve damage from the surgical IV on the left. “No problem,” she replies. She places a fingertip on a vein below my right elbow, and then wraps a turquoise rubber tourniquet above the elbow. She reaches into a slim drawer, which is the only aspect of blood collection, at this point, that makes me flinch, as she pulls out a dark, stainless-steel twenty-two-gauge needle, plainly visible inside of a disposable syringe. “You can make a fist,” she directs. When I do, she says, “It’s okay,” and pats my forearm, indicating I should ease up a bit. She presses the needle to the skin, and says, “Okay, a little stick.”
With the line in, she again pats my forearm, and says, “It’s okay. I know you had a bad experience.” I don’t know if she is referring to the surgical IV or the two failed cycles.
In half an hour, Derek and I will sit in the small park across the street and eat toasted bagels with cream cheese. Three boys, who seem to be siblings, will glide by on Razor scooters. One week later, I will read Jane Brody’s article and feel naïve for believing I still had the choice—time, regardless of any regrets, has always seemed to replenish itself. There is no way to reach back and affect time—to opt out of the bad relationship sooner, to meet Derek sooner, to think about egg reserve and egg quality sooner. The choice I do still have is to not resurrect moments of embarrassment and disappointment to generate regrets.
Joshua Tree National Park / photo by Derek Wright
Poet and philosopher David Whyte describes a kind of border, between what we envision for ourselves, and reality, our desires and imaginings in constant conversation with reality. In that liminal space, we have as much of a chance of affecting our reality as it does of affecting us, he suggests. For me, recognizing the distinction between the image I’ve had of my future and the realistic circumstances of my timeline spurs some other kind of chemistry, and I am rushed into the present.
Christina slips off the tourniquet with one hand, and, with that same hand, swipes her palm down my inner arm and gently opens my fingers, which are still clenched in a fist. I am grateful for her kindness and care, though in a month I’ll start over again—I could not quite yet, it seems, abide the dark, echoic landscape of my ovaries on screen during an ultrasound.
When I eventually do reaffix the estrogen patch, the curtains in my bedroom are closed, the morning light muted behind beige canvas. I peel off the adhesive, and press the patch to my lower abdomen for ten seconds. I move with gentleness and precision, like Christina, and in a few brief and solitary moments in a dark and quiet room, it is again ordinary to want this. I remember looking at Christina after she smoothed open my fingers—I’d smiled, and said, Thanks, have a good rest of your day , feeling intact. Total certainty is a rarity. But there is room for softness, nonetheless.